Personalized Medicine or Precision Medicine consists of adapting medical therapies to individual characteristics of each patient. In the context of Medical Cannabis, individualizing treatments is essential for effective results. After all, in addition to a unique biochemical structure,Personalized Medicine or Precision Medicine consists of adapting medical therapies to individual characteristics of each patient. In the context of Medical Cannabis, individualizing treatments is essential for effective results. After all, in addition to a unique biochemical structure, each individual has a unique Endocannabinoid System (ECS)..
Research on ECS gained strength in the second half of the 20th century, although the therapeutic use of the plant is an ancient practice. The scientific apparatus helps in the deconstruction of stigmas that make it difficult to consolidate the medical use of cannabinoid derivatives in several countries. In Brazil, the recent regulation of Medical Cannabis by the Anvisa has awakened the medical community to the subject.
In this content, we are going to talk about this scenario, correlating Medical Cannabis and the stimulus to a personalized medical practice from individualized prescriptive strategies. Read on and understand why the therapeutic use of cannabinoid derivatives has been consolidating in different fields, in several parts of the world.
The use of cannabinoids and personalized medicine
In recent years, there has been a remarkable paradigm shift in medical practice towards personalized and preventive medicine, consolidating a gradual, consistent and global movement that proposes a truly integrated approach to health care.
This approach combines scientific apparatus from different fields in Medicine and biomedical technologies. Thus, using the individual characteristics of each patient, such as clinical, genetic (referring to specific genes) and genomic (referring to the entire DNA) data, it is possible to select increasingly safer and more effective treatments.
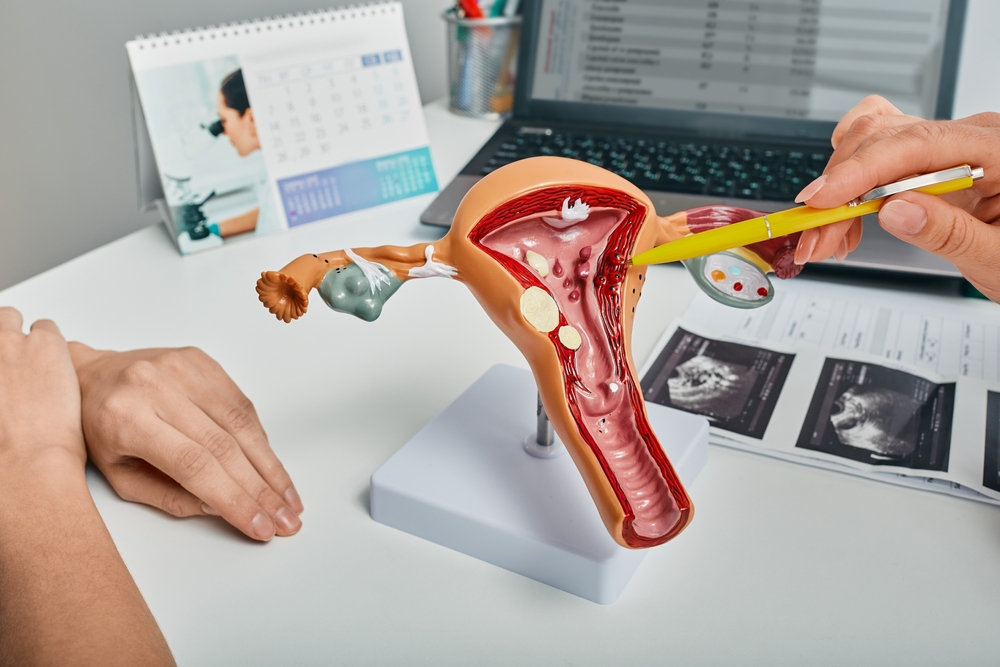
The practice of Endocannabinoid Medicine is fully aligned in this context of personalized and integrated Medicine, since a successful prescriptive practice always depends on the individualization of therapeutic strategies, since each of us has a unique biochemical structure and, therefore, an unique Endocannabinoid System.
The complexity of cannabinoid compounds, as well as each individual’s genetic predispositions – que modulam como cada paciente metaboliza esses compostos – which modulate how each patient metabolizes these compounds – leads to a wide range of physiological responses to this therapy. The ideal strategy is, therefore, one that identifies the most appropriate formulation, dose and dosage to meet each patient’s individual needs.
Due to their broad spectrum of action, cannabinoids are a valuable tool in dose reduction and drug weaningavoiding adverse effects arising from polypharmacy. Compared to single-molecule drugs (often prescribed for chronic pain, anxiety or depression, for example), medical cannabis, when used assertively, tends to bring more comprehensive results, encompassing different symptoms and treating them concomitantly.
> For more information on assertive prescriptions, read this Guide: How to dose cannabinoid derivatives..
Why pay attention to this scenario?
For its broad therapeutic potential extensively explored by Science – in more than 27,000 scientific papers published on PubMed – medical Cannabis has awakened the interest of the medical and scientific community.
In Israel – one of the reference countries in the regulation of the medical use of Cannabis in the world – the prescription of cannabinoid derivatives is a common practice for conditions of chronic pain and other clinical settings often refractory to common therapy. A survey carried out on 64% of all pain specialists in the country shows that the majority of them prescribe Cannabis..
See more survey data:
- 63% found cannabis moderately to highly effective,
- 56% found mild or no side effects, and
- only 5% found it to be significantly harmful.
The most common indications are for:
- neuropathic pain (65%),
- cancer pain (50%),
- arthralgias (25%) and
- any type of pain considered as intractable (29%).
>> Read the full study here: Personal experience and attitudes of pain medicine specialists in Israel regarding the medical use of cannabis for chronic pain.
The work concludes that physicians experienced in prescribing cannabis for a prolonged period, see the treatment as an effective and safe option for chronic pain.
Their answers suggest a possible paradigm shift from using cannabis only as a last resort and being in line with what several other doctors, researchers and authors are discovering in relation to the chronic use of said compounds: improved quality of life in patients suffering from chronic, refractory and disabling diseases. As this research below shows, which followed 10,000 patients on regular use of medical cannabis over a period of 6 mounths.
Supervised and individualized therapy with medical cannabis is associated with high adherence, improved quality of life and decreased pain level, with a low incidence of major adverse events..
>> Read the full study here: Adherence, Safety, and Effectiveness of Medical Cannabis and Epidemiological Characteristics of the Patient Population: A Prospective Study
The more scientific research evolves, the more the medical community and patients have access to the therapeutic potential of this drug class.
Physicians who wish to incorporate this vast therapeutic arsenal into their medical practice must seek appropriate education in the field to ensure safe and effective prescribing.
The WeCann Academy helps you to get ready for this scenario. We connect experts from all around the world, in a global community of studies and research in the Endocannabinoid Medicine, sharing scientific knowledge and practical experience.
Do you want to take part in this community? Contact us and learn more about it!
References
Bar-Lev Schleider Lihi, Mechoulam Raphael, Sikorin Inbal, Naftali Timna, Novack Victor. Adherence, Safety, and Effectiveness of Medical Cannabis and Epidemiological Characteristics of the Patient Population: A Prospective Study. Frontiers in Medicine, v. 9. 2022
Bonn-Miller MO, ElSohly MA, Loflin MJE, Chandra S, Vandrey R. Cannabis and cannabinoid drug development: evaluating botanical versus single molecule approaches. Int Rev Psychiatry. 2018.
Golubnitschaja O, Baban B, Boniolo G, Wang W, Bubnov R, Kapalla M, Krapfenbauer K, Mozaffari MS, Costigliola V. Medicine in the early twenty-first century: paradigm and anticipation – EPMA position paper 2016. EPMA J. 2016.
Sharon H, Goldway N, Goor-Aryeh I, Eisenberg E, Brill S. Personal experience and attitudes of pain medicine specialists in Israel regarding the medical use of cannabis for chronic pain. J Pain Res. 2018.